Clinical

Time for action on obesity
In Clinical
Bookmark
Record learning outcomes
The UK population is more obese and less active than ever before – so much so that in some parts of the country, life expectancy is actually beginning to drop. Can pharmacists help turn things around?

Learning objectives
After reading this feature you should be able to:
• Explain the findings of the latest Health Survey for England
• Approach customers about the possibility of supporting them to lose weight
• Help customers by advising on those weight loss products best suited to their individual goals and needs
The latest Health Survey for England (published December 2018) found that the overwhelming majority of adults are so unhealthy they are actually putting their lives at risk. The survey questioned 8,000 adults and 2,000 children about a variety of topics including obesity, smoking and drinking.
Despite Government warnings about the risks of obesity-related illnesses such as diabetes, heart disease and cancer, waistlines continue to expand. Just over a quarter of adults are now classed as clinically obese and, according to a House of Commons briefing paper, one in 10 children is obese by the age of five years, rising to one in five by the age of 11 years.
Over-eating, an unhealthy diet loaded with sugar and fats, and a lack of exercise are typical reasons why people are piling on the pounds. However, Professor Mahendra Patel, a Royal Pharmaceutical Society board and assembly member, says there are other common causes for people being overweight, including having an underactive thyroid, metabolic syndrome, stopping smoking and genetics, where you may inherit your family’s tendency to gain weight. Weight gain can also be the result of taking certain medications, such as when treating diabetes or epilepsy.
With obesity levels showing no signs of decreasing, pharmacists can play “a pivotal role in supporting people to lose weight and to take on board a healthy lifestyle”, says Professor Patel.
Starting point
As a starting point to helping customers lose weight and maintain a healthy lifestyle, it is useful for pharmacists and their teams to be aware of the early biological changes and behaviours that lead to obesity. The latest Health Survey for England found that one indicator of obesity in children can be if their parents are obese.
NHS Digital says the survey has revealed for the first time that children of obese parents are more likely to be obese themselves than children whose parents are not overweight or obese. The survey showed that 28 per cent of children of an obese mother were also obese, compared with 8 per cent of children whose mother was not overweight or obese.
Twenty-four per cent of children of an obese father were also obese, compared with nine per cent of children where the father was not overweight or obese.
Dr Max Davie, officer for health promotion for the Royal College of Paediatrics and Child Health (RCPCH), says the link between parent and child obesity is “a cycle of life that can have terrible consequences for the health of entire families for generations”.
To address this issue he calls for “specialist weight management services for overweight and obese families, supporting parents to lose weight before conception. We need services in place to continue this support throughout pregnancy and childhood”.
Children are reliant on caregivers for their nutrition. Eating and lifestyle habits tend to be established early in life, “so it is important that the whole family sets an example by adopting a healthy, active lifestyle”, says Dr Stacey Lockyer, nutrition scientist at the British Nutrition Foundation.
A family’s approach to what constitutes a healthy lifestyle will vary, however, and research has shown that children from lower socio-economic backgrounds are more vulnerable to poor nutrition and being overweight.
A study published in The Lancet (March 2018) found that despite numerous policies to tackle obesity, their effects had been “insufficient in preventing the emergence and widening of BMI inequalities in childhood and adolescence from 1953 to 2015”. The study also highlighted the “powerful influence of the obesogenic environment” that had “disproportionately affected socio-economically disadvantaged children” during that period.
The study recommended the need for new approaches, particularly given the absolute increases in BMI inequality with age. “Without effective intervention, these inequalities are anticipated to widen further throughout adulthood in future cohorts,” researchers said.
Dr Lockyer says children who are overweight or obese are “disproportionately from low-income households”. Likely reasons for this, she says, include the fact that “deprived areas of the UK tend to have a higher density of fast food takeaways and there may be other issues such as a lack of green spaces or safe walking and cycling routes”.
Where obesity was once regarded as being more predominant in affluent individuals, the rise in obesity among low income households could be because “cheap junk food”, full of sugar and salt, is “readily available and cheaper, making it easier for people with less money to consume”, says Mahendra Patel.
When working long hours, a cheap take-away for the family can be more appealing and less time-consuming than cooking a well balanced meal – and some families might lack the knowledge about what constitutes a healthy meal through a lack of education about nutrition, suggests Lila Thakerar, superintendent pharmacist at Shaftesbury Pharmacy in Harrow.
Key facts
- Children of obese parents are more likely to be obese themselves
- A family’s approach to what constitutes a healthy lifestyle will vary
- New digital technologies can be used to maintain a healthy weight pharmacist at Shaftesbury Pharmacy in Harrow.
Right approach
Approaching customers about the possibility of supporting them to lose weight should be done sensitively and be based on individual needs. Any approach regarding weight management can also “depend on the rapport you have with individual customers”, Professor Patel says.
He suggests initial conversations with customers can include signposting to local and regional organisations, in addition to giving advice and support about healthy living and nutrition as a way of encouraging people to consider ways of managing their weight.
Placing posters and leaflets advertising weight loss services and the value of having a healthy lifestyle by the pharmacy counter can encourage customers who may be too embarrassed to discuss their concerns to start a conversation. “We have lots of leaflets on our counters to encourage people to start a conversation about their diet,” says Lila Thakerar.
Prevention is also an important part of managing weight and encouraging a healthier lifestyle, which has been highlighted in the NHS Long Term Plan. Most pharmacies now have healthy living status so, as well as focusing on helping people to achieve a healthy weight, they can also be given advice about exercise alongside other lifestyle issues such as smoking cessation and alcohol consumption, she says.
One of the advantages of pharmacy is that weight management support for families can be offered on a regular and flexible basis. Weight loss is often an extremely sensitive subject for people, so the consultation room can be a place where they can talk about their issues in confidence.
Deprived areas of the UK tend to have a higher density of takeaways
Mahendra Patel agrees that, as most community pharmacies have healthy living status, pharmacists and their teams are now appropriately skilled and trained to talk to patients about conditions such as weight management and to deliver effective “healthy lifestyle messages”.
The key to helping customers take control of their weight is to provide them with the kind of one-to-one support that pharmacies are well placed to deliver. For example, pharmacists can set up a weight management service for the local community. When talking to customers it is important to find out what they’ve tried, what they hope to achieve and what will work for them, so they feel they have ownership of their weight loss programme.
Ethnic minority groups from the South Asian sub-continent are particularly vulnerable to heart disease, stroke and type 2 diabetes associated with obesity, says Professor Patel. He advises pharmacy to “play a bigger part engaging with these communities about healthy lifestyles more effectively – and it is an opportunity to add to the Government’s healthcare and prevention agenda and the new NHS Long Term Plan”.
Pregnancy and nutrition
Pharmacy teams can help improve the public’s understanding of how the environment can influence parents’ and children’s behaviours regarding nutrition and weight management, even before birth. Research has shown that past this point, damage could be irreversible.
Lila Thakerar, superintendent pharmacist at Shaftesbury Pharmacy, Harrow, finds many pregnant women “eat for two”, which can lead to weight problems. “There is a misconception that you need to eat for two rather than eating healthily and can put on weight that is not just baby weight but your own weight as well.
“Pregnant mothers need to be aware of weight issues. They can become overweight and some also have the misconception that a chubby baby is a healthy baby,” she says. Pharmacies can help by signposting pregnant women and those who have just given birth to guidance about weight management and nutrition from their midwives and health visitors, she advises.

Wide choice
From cereal bars and shakes to herbal tablets and prescription-only slimming drugs, customers have many choices when it comes to products to help them lose weight. Faced with so many options, pharmacy teams can help by advising on those products best suited to individual weight loss needs. And by developing a supportive relationship with customers, pharmacists can not only boost weight loss, but also encourage loyalty and increased sales as well.
New digital technologies can be used to maintain an optimum weight and help families achieve healthy, sustainable lifestyles. Pharmacy should “continue to move with the times”, Professor Patel says, and signpost people to the wide range of apps on offer to help people get healthy, including fitness trackers, weight loss plans and calorie checkers.
And as not everyone has a smart phone, pharmacies can also direct customers to online information, such as the NHS website, which includes a whole range of healthy eating plans, or to podcasts that feature fitness advice. Change4Life also provides plenty of resources that can be used by parents to help them make healthy food choices for their families.
Food labelling
While technology is in place to help tackle the obesity crisis, other measures need to be taken to address what is causing it – and the spotlight has been on the food industry for some time.
In June 2018, the Government published the second part of its plan for action on tackling childhood obesity. Just months later (November 2018) the Obesity Health Alliance (OHA) issued an analysis that revealed 43 per cent of all food and drink products in supermarket hot spots were for sugary foods and drinks. Displaying unhealthy products in areas such as store entrances, ends of isles or at the tills can encourage shoppers to buy more of these products, says the OHA.
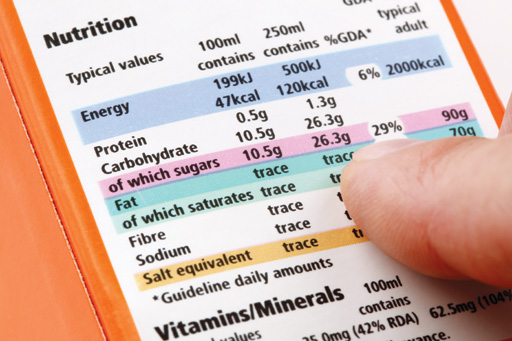
Lila Thakerar believes it is time the Government held the food industry to account for contributing to the obesity crisis. “For example, there is so much confusion about the labelling of food products. I go for low sugar products, yet I look at the label and the product has got loads of fat. Meanwhile, low fat products can have enormous sugar content. It is very confusing for customers. All products should be clearly labelled,” she says.
Weight management top tips
- Offer a range of weight loss options and services that suit customers’ requirements
- Provide customers with one-to-one advice about healthy living to support them in their weight loss aims
- Ensure goals are realistic
- Signpost people to sources of healthy living advice, including digital technology
- Promote healthy living messages more widely in the community by working with local schools and clubs

Other options
As well as looking at labelling, the Government has also been considering ways that food taxes and marketing restrictions can be used as a means of tackling soaring obesity rates. As part of the childhood obesity plan it is currently consulting on several strategies in this area, including:
- Banning the sale of energy drinks to children
- Further limiting children’s exposure to advertising of foods high in fat, salt and sugars
- Banning price promotions, such as ‘buy one get one free’ and multi-buy offers or unlimited refills of unhealthy foods and drinks
- Banning the promotion of unhealthy foods and drinks by positioning at checkouts, the ends of aisles and store entrances.
A soft drinks industry levy is in force aiming to reduce sugar consumption, and the food industry has been given voluntary targets to reduce the sugar and calories in certain food categories that contribute the most to excess energy intake in children.
The Government is also looking at using Healthy Start vouchers to provide additional dietary support to children from lower income families and Dr Lockyer explains it is developing “a trailblazer programme” with local authority partners to show what can be achieved in communities to tackle childhood obesity.
While “taxing certain products, such as sugary drinks, is fine… putting a couple of pence on sugary drinks may not necessarily make much difference to a great many”, says Mahendra Patel. There are “no quick fixes”, he points out, and the Government needs to find better ways to engage with people by offering simple messages about health and lifestyle.
Some families might lack knowledge of what constitutes a healthy meal
Simplicity works
The ‘5 A Day’ campaign has had a powerful impact because of its simplicity, he says. Patel suggests making health messages more pictorial – such as showing the amount of sugar in a cereal using an image of sugar cubes on a spoon.
While pharmacy can help to get across important but simple health messages, he cautions against “over preaching” to people, saying pharmacies should “set people realistic weight loss goals, evaluate their progress and explain healthy options tailored to meet individual needs”.
Pharmacists are based in the heart of communities and easily accessible, he says, so have an opportunity to spread the word about good nutrition and weight management more widely by working with organisations, such as schools and local clubs, to promote healthy living messages much more effecti

