The best advice that can be provided to a parent is to help them understand they are not alone and there are some simple steps they can follow to make managing the bedwetting easier for both them and their child.
Being prepared - one of the simplest ways to manage bedwetting is to be as prepared as possible. Laying out a spare set of bedsheets and pyjamas next to the bed can help a parent respond very quickly to a bedwetting incident and with minimum fuss, especially if it is in the middle of the night, thus ensuring everyone gets back to sleep quickly. Placing a protective bed mat s on to the mattress is another tool to protect against accidents as they provide a layer of absorbent protection on the bed which can be removed quickly. The use of waterproof sheets or duvet covers can help reduce long term damage to beds and mattresses.
Absorbent sleep wear - an absorbent product can be a useful support particularly for older children who will have been out of nappies or training pants for some time. These are particularly useful to help build a child's confidence to deal with bedwetting by reducing any worry or anxiety, for example, if they are going to a 'sleep-over' with friends or away on a school trip. It may be thought that wearing absorbent sleepwear means the bedwetting issue is not being addressed and consequently delay or hinder the child's progress. In reality, there is no evidence to suggest this is the case, and the products just discreetly help manage the bedwetting.
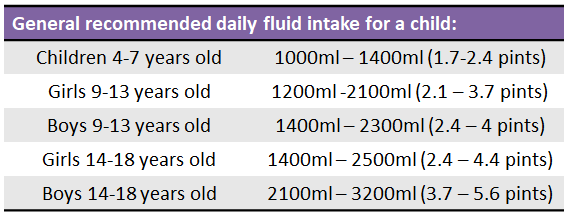
Fluid intake - a parent may assume that if their child were to drink less then there is a strong likelihood they will wet the bed less. This is not the case and restricting fluids could not only dehydrate the child but contribute to making the problem worse. Dehydration causes the production of concentrated urine that may be irritant to the bladder, triggering urination. Some children may even have a smaller than average bladder capacity resulting in frequent trips to the toilet during the day or night. Gradually increasing the amount the child drinks in the day could help increase the volume the bladder can hold.
 (Source: NHS Choices)
(Source: NHS Choices)
These amounts can vary dependent on a child's diet and levels of exercise, and some children may not need this much. It is advisable that this increased fluid intake is not in the form of sugary drinks as these may adversely impact the child's health, or drinks that contain caffeine such as cola, coffee or energy drinks as caffeine is a diuretic that will increase the volume of urine and consequently the need to urinate.
A parent may question if they should limit fluid intake at night in particular. It is suggested that the majority of the recommended fluid intake should be drunk during the day and reducing drinks an hour before bedtime may help with bedwetting, however a child should never be refused a drink if they are thirsty.
Toilet habits - encouraging a child to use the toilet frequently during the day will assist with bedwetting, anywhere between four to seven times is normal with the final time just before going to bed. Many parents may at some point attempt to carry a sleeping child to the toilet at night to stop or control the bedwetting. This can actually be counterproductive as it will reinforce to the child that they can urinate whilst asleep and not respond to their brain waking them because of a full bladder. A more productive strategy would be to remove any barriers to enable a child to be able to get to the toilet easily when the urge arises. So for example, if the child sleeps in a bunk bed they should be encouraged to sleep in the bottom bunk so they can get out of the bed easily or leave a light on so they can see their way to the bathroom.
Addressing missed signals - if a child is not yet able to respond to the signal of a full bladder there is an option of using a bedwetting alarm or buzzer which alerts them if they begin to urinate and encourages them to get up. These can be motivating in children over the age of 7 and can be particularly useful for children who sleep heavily. Bedwetting alarms are not prescribed on the NHS, but are available to purchase online from the children's continence charity ERIC (Education and Resources for Improving Childhood Continence).
Reassure and reward the child - providing reassurance to the child at all times is recommended. Although it can be both frustrating and tiring for a parent to deal with bedwetting it is important not to punish the child for any bedwetting incident as this can place the child under further stress and anxiety which could even make the problem worse. Just like potty training, reward schemes can be motivating for some children to help management strategies be more effective. The rewards should not be based on the child not wetting the bed though as this is something out of their control. Instead rewarding positive behaviours is advised, such as when the child remembers to go to the toilet before bed, or sticks to the amount they are asked to drink during the day.
