Time to quit smoking
In OTC
Follow this topic
Bookmark
Record learning outcomes
Smoking rates are on the decline across the UK, with more and more people setting quit dates, but there’s still a long way to go to protect the nation’s health
Some 14.1 per cent of adults in the UK smoked cigarettes in 2019, equating to around 6.9 million people, which is down from 14.7 per cent the year before. This is according to the latest figures from the Office for National Statistics (ONS), published in July 2020. However, the report shows that smoking rates continue to vary around the country, as 15.6 per cent of adults in Northern Ireland smoke, compared to 15.5 per cent in Wales, 15.4 per cent in Scotland and 13.9 per cent in England.

Despite overall numbers of smokers decreasing, smoking prevalence still remains concentrated among certain groups in the UK. For example, 15.9 per cent of men smoked in 2019 compared with 12.5 per cent of women, and 23.4 per cent of people in routine and manual occupations smoked in 2019, which is around 2.5 times higher than people in managerial and professional occupations (9.3 per cent).
Groups where smoking prevalence is higher “include disadvantaged groups and communities including people with mental health conditions, those who are unemployed or on low incomes, LGBTQ+ communities and certain BAME communities,” says a Public Health England (PHE) spokesperson. “In addition, the prevalence of women smoking throughout pregnancy has remained relatively stable for a number of years, with around one in 10 babies born to a mother who smokes. Smoking in pregnancy is strongly associated with low socioeconomic status.”
Support services
Many smokers want to quit but aren’t sure how to do so, and while general information is available online, some still prefer one-to-one advice. A survey in May 2020 by Asthma UK and the British Lung Foundation revealed that most smokers looking to quit have said they wouldn’t want to quit ‘cold turkey’. Two-thirds of people planning to quit use some form of support or aids recommended by healthcare professionals, such as nicotine patches, e-cigarettes and behavioural support. Crucially, more than a quarter of smokers with lung conditions say they would consider turning to the NHS for support.
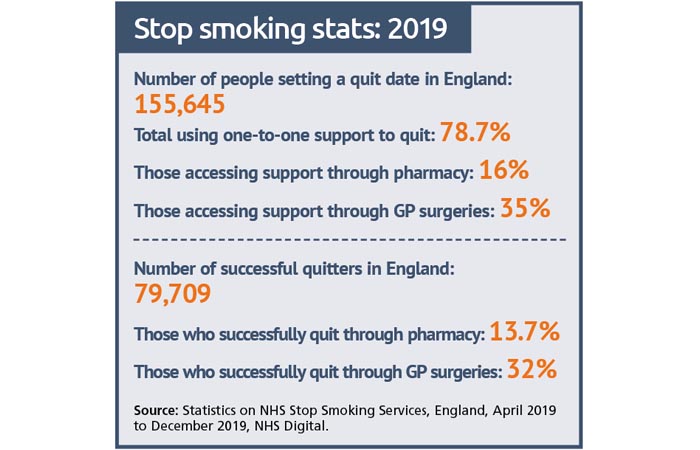
Research show that smokers are three times as likely to quit successfully if they use a combination of medication and specialist support from a local stop smoking service. According to NHS Digital, between April and December 2019, approximately 78.6 per cent of smokers in England who set a quit date used one-to-one support to help them quit smoking, with just over 16 per cent using stop smoking support through pharmacy. However, the uptake of stop smoking services has been declining overall in recent years.
“There are a number of factors involved in the reduction in the number of smokers accessing local stop smoking services in England, including lack of efficient referral routes and decommissioning of services in some areas,” says a PHE spokesperson. “However the overall effectiveness of these services remains high and there is some evidence of an increase in demand from smokers since the outbreak of the coronavirus pandemic, with smokers feeling more motivated to quit in order to improve their health. Proactive initiatives such as text messages from GPs to patients who smoke, encouraging them to seek quitting support from their local service, have achieved good results in engaging smokers.”
A survey by public health charity Action on Smoking and Health (ASH) in May 2020 found that within a month of lockdown, most councils had services in place to help smokers quit, and around a quarter reported an increase in people seeking help to quit. This followed PHE guidance to smokers, after research revealed that smokers could be at risk of more severe Covid-19 symptoms. Some 96 per cent of local authorities reported that smokers still had access to support from a trained advisor and 88 per cent reported that smokers could still access medications or e-cigarettes via the services. In addition, 24 per cent reported that they had seen an increase in people seeking support.
According to PSNC, since smoking prevalence is highest in deprived communities, stop smoking services should be easily accessible in these areas. Hazel Cheeseman, director of policy at ASH, says that in the last few months these services have had to radically re-orientate themselves and move over the phone and online. “Early feedback is that this new way of working has some advantages, but it also poses challenges, particularly in terms of access to medication and in reaching groups less comfortable receiving support in this remote fashion,” she says. “The role of pharmacists has never been more important, from ensuring that medication can still be accessed to picking up on those smokers who perhaps don’t want to engage with telephone support.”
Some 14.1 per cent of adults in the UK smoked cigarettes in 2019, equating to around 6.9 million people
Conversation starters
In 2015, a survey of over 2,100 adults revealed that 67 per cent of smokers are comfortable accessing stop smoking services from their local community pharmacy. In addition, according to PSNC’s ‘Think Pharmacy’ campaign, there’s a strong evidence base for the effectiveness of pharmacy-led stop smoking programmes. Pharmacy staff routinely have contact with people who are in good health, as well as those visiting a pharmacy due to illness, and are accessible to people of all ages, including younger people and anyone who use more formal healthcare settings infrequently, such as men.
PHE has found that quitting motivation has been high during the Covid-19 pandemic. “The UCL Smoking Toolkit Study finds that around one in seven smokers in England who made a quit attempt last year were successful, while this year the success rate has risen above one in five,” says a PHE spokesperson. “So, while in 2019 fewer than one in 20 smokers reported having quit in the previous year, this year the rate is closer to one in 12.”
Hazel says that since people are particularly concerned about their health and want to make a change, pharmacy teams should seize this moment to publicise smoking cessation services, advice and support. “If you smoke, there are few other things you can do today that will improve your health tomorrow,” she says. “Smokers are receptive to the message that they can and should improve their health at this time. We have heard from a number of quit services that say numbers quitting are up and success rate is up. This has proven to be a real teachable moment.”
According to PHE, pharmacy teams have a variety of opportunities to discuss smoking, such as when people are repeatedly buying nicotine replacement products (NRT) or cough medicines, or when dispensing medicines for smoking-related conditions such as high blood pressure, chronic obstructive pulmonary disease (COPD), diabetes and heart disease. Teams should ensure they make every contact count and talk to customers about available quitting approaches and support, as well as helping to promote smoking cessation campaigns such as Stoptober (throughout October) and No Smoking Day (in March).
“All members of the pharmacy team should offer very brief advice (VBA) on smoking, based on the model ‘Ask, Advise, Act’, and recommended by NICE,” says a PHE spokesperson. “The National Centre for Smoking Cessation and Training (NCSCT) provides a free online training module on how to deliver VBA. Staff should know about the specialist quitting support available locally and should also ensure their knowledge of all quitting options and their effectiveness is up to date – see [the Government’s] ‘Health Matters: Stopping smoking – what works?’ [guidance document]. Public Health England has published Covid-19 advice for smokers and vapers, which encourages smokers to quit smoking to improve their health.”
Pharmacy offerings
PHE recommends three ways to quit smoking alongside one-to-one support: Champix (varenicline) and Zyban (buproprion) on prescription, or using NRT products, which are available on prescription and over the counter. NRT products are suitable for most adults, but customers with a heart or circulatory condition, or those taking regular medication, should check with their doctor first. Pregnant women should also consult their doctor or midwife before using NRT.
“Using NRT products bought over the counter makes it one and a half times as likely a person will quit smoking successfully,” says a PHE spokesperson. “Using a combination of products – a slow-acting nicotine patch plus a fast-acting product such as gum or lozenges – increases the effectiveness. Structured behavioural support from a healthcare professional increases effectiveness further and is the gold-standard treatment. As pharmacy staff already know, there is often misunderstanding of the harmfulness of nicotine, with four in 10 smokers and ex-smokers incorrectly thinking that nicotine causes most of the smoking-related cancer. Given these inaccurate perceptions, advising on the relative safety of nicotine-containing products compared to smoked tobacco is an essential part of supporting them to quit.”
Some people may prefer to use e-cigarettes rather than licensed NRT products. According to the recent ONS data, 5.7 per cent of respondents said they used an e-cigarette in the UK in 2019, which equates to nearly three million adults. The most common reason given for vaping was as an aid to stop smoking, with approximately half (50.6 per cent) of vapers reporting using e-cigarettes for that purpose in 2019. A major UK randomised control trial found e-cigarettes to be twice as effective as NRT products when combined with behavioural support. According to PHE, pharmacy teams should update their knowledge on the evidence and products available and should provide advice in line with NICE guidance NG92.
“The pharmacy sector has had an up-and-down relationship with vaping products over the years,” says Dan Marchant, director at Vape Club and founding member of the UK Vaping Industry Association. “But I believe now is definitely the time for them to fully embrace the category. Although these are not medicinally licensed products, they absolutely sit within the pharmacy category, alongside the more traditional NRT products, and are well regulated in the UK. Most people tend to trust their pharmacist implicitly... If pharmacies were to offer a comprehensive range of smoking cessation vaping products, these customers will be coming back every week to top up on their supplies.”

Most smokers looking to quit have said they wouldn’t want to quit ‘cold turkey’
Teen smoking trends
In May 2020, new anti-smoking laws banned the sale of menthol-flavoured cigarettes in the UK. It’s too early to assess any impact of this ban on smoking rates, but ASH said this was long overdue and welcomed it as an essential next step towards ending the tobacco epidemic. Menthol cigarettes are often seen as a child-friendly starter product because the menthol makes it easier to smoke and to inhale the smoke deep into the lungs. Menthol smokers are also more likely to become heavily addicted and find it harder to quit.
A new analysis of child smoking rates by the All Party Parliamentary Group on Smoking and Health showed how the number of children aged under 16 taking up smoking fell dramatically as Government regulation of tobacco tightened after the turn of the century. Around one in five children smoked throughout the 1990s and now fewer than one in 20 children smoke. However, 280 children still light up for the first time every day, so there’s no room for complacency. Two thirds of those experimenting with smoking go on to become daily smokers.
Hazel says the most effective way to reduce youth smoking is to change the adult environment. “Ending almost all tobacco marketing has had a significant effect over time on youth smoking rates, for example,” she says. “One of the most important factors in youth uptake is parental smoking. Getting parents to quit when they conceive and stay quit as their children grow up has massive health gains in terms of protecting children from secondhand smoke and reducing the likelihood that they will start smoking in their teens.”
See more informaton on smoking and vaping in this pharmacy scenario.
Quitting in 2020

In July 2020, Action on Smoking and Health (ASH) and University College London (UCL) surveyed 1,370 smokers and recent ex-smokers through the YouGov Covid-19 Tracker.
The analysis found that over a million people in the UK had stopped smoking since the Covid-19 pandemic hit the country, while a further 440,000 smokers tried to quit during this period. Younger smokers aged 16-29 (around 400,000 people) were more likely to quit than those aged over 50 (240,000 people).
“The difference in rates of quitting between age groups is quite astonishing,” says Dr Sarah Jackson, behavioural scientist at UCL. “Older smokers don’t seem to have responded to the coronavirus pandemic in same way as younger smokers. However, we know younger smokers tend to struggle more with relapse and those who feel they might go back to smoking should look for support to stay quit.”
Among smokers aged under 30, seven per cent said they had quit as a result of Covid-19, while only three per cent of smokers over 50 had quit for this same reason. Younger smokers may also have been prompted to quit due to income changes, moving back to the family home and/or a disruption to their social life tied into smoking-related settings such as pubs, bars and parties.
A new campaign, funded by the Department of Health and Social Care, has been launched to call on people to quit smoking, especially older smokers who may be more at risk of Covid-19. Research shows that smokers have an increased risk of contracting Covid-19 and are more likely to have severe symptoms, possibly because they are more likely to have underlying smoking-related conditions such as chronic obstructive pulmonary disease, diabetes, stroke and other heart conditions.
