Four nations women's health overview
England
According to Women's health strategy England although women in the UK on average live longer than men, women spend a significantly greater proportion of their lives in ill health and disability when compared with men. Not enough focus is placed on women-specific issues like miscarriage or menopause, and women are under-represented when it comes to important clinical trials. This has meant that not enough is known about conditions that only affect women, or about how conditions that affect both men and women impact them in different ways. The Women's health strategy published in 2022 covers a 10 year women's health strategy for England.
During 2023 a range of new actions relating to women's health were launched in England including:
- Between launch on 1 April and 31 December, 484,082 HRT prescription prepayment certificates were purchased, saving women millions of pounds in ongoing prescription charges
- NHS England announced its ambition to eliminate cervical cancer by 2040 by making it as easy as possible for women to get the lifesaving human papillomavirus (HPV) vaccination and increasing cervical screening uptake
- The NHS England Pharmacy Contraception Service relaunched to enable community pharmacies to initiate oral contraception. Almost 3,000 pharmacies have already signed, making access to contraception easier
- Between launch in July 2023 and early January 2024, there were 102,872 visits to the new women’s health area on the NHS website and 1.26 million visits to its new hormone replacement therapy area
- In September 2023 improvements were made to IVF transparency through an accessible new tool on GOV UK to allow people to look up information about NHS-funded IVF treatment in their area
There have been various cross-government initiatives to support women in the workplace, including:
- Appointing recruitment and employability expert Helen Tomlinson as the government’s Menopause Employment Champion to improve support for menopause in the workplace
- The government announced £12.4 million to help change choices about work, which included 6 ground-breaking projects including an investigation looking at how endometriosis impacts women in the workplace
Wales
In November 2022 NHS Wales published a document entitled Women's Health in Wales and the following actions were identified:
- Develop actions, key deliverables, and measurable outcomes from the six priority improvement opportunity areas set out in this discovery report.
- Identify and embed techniques and behaviours that ensure women’s and girls’ voices are heard in every interaction they have with the NHS.
- Provide prompt access to help and support across the health system.
- Develop better workplace and mental health support, enabling increased uptake of self-care and lifestyle management, and enhance support to cope with the health and wellbeing consequences of being parents and carers.
- Enhancing and providing easier access to high quality information resources.
- Pioneer best practice and providing advice and guidance on how the workplace can support wellbeing, work/life balance and mental health.
- Carry out qualitative and mixed methods research on key topics that support the needs of women and girls.
The NHS Wales Executive also stated "Although women and girls make up over half of the Welsh population, women’s health and wellbeing is often undervalued and under-resourced and there is a need to reduce health inequalities, improve equity of service and improve health outcomes for women in Wales.
Inequalities in health outcomes exist between both men and women and between different groups of women in Wales. We must work to reduce health inequalities that women experience when it comes to diagnosing and treating ischaemic heart disease, cardiovascular disease, screening for cancers, and other major health conditions. Health inequalities in different groups of women, in different parts of Wales are unjust and preventable.
We can reduce some health inequalities by identifying gaps in health service provision, considering areas of best practice, and developing actions to address these gaps, tailored to meet the needs of all women.
It is important to note that health inequalities are socially determined by a set of factors and circumstances and these circumstances can disadvantage people and limit their chance to live longer, healthier lives.
These factors cannot be solely addressed by the Women’s Health Plan, however improving access to health services has an important role to play in reducing health inequalities".
Scotland
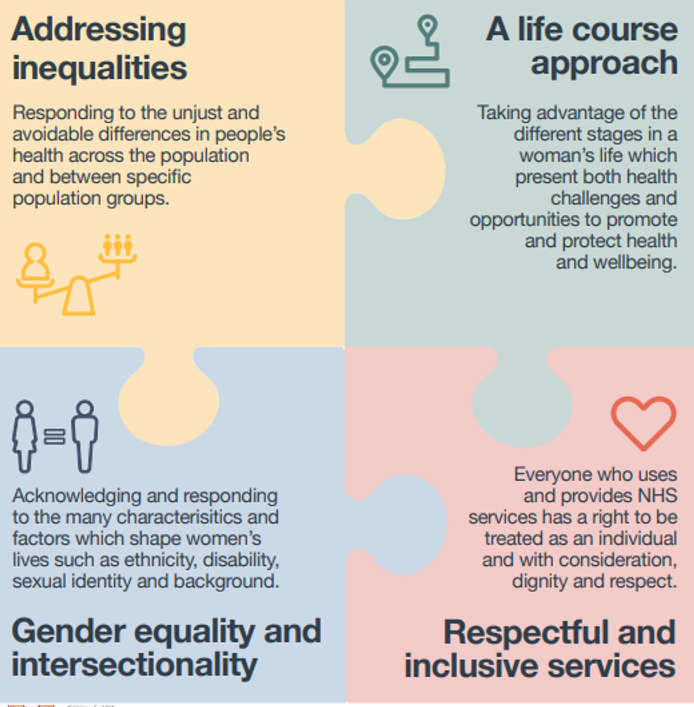
On 20th Aug 2021 Scotland's Women's health plan states that "The Women’s Health Plan underpins actions to improve women’s health inequalities by raising awareness around women’s health, improving access to health care and reducing inequalities in health outcomes for girls and women, both for sex-specific conditions and in women’s general health". The work on the Women's Health Plan began before the pandemic – and the evidence was already stark about the inequalities impacting women's health, so actions were raised. This was relating to the Women’s Health Plan A plan for 2021-2024 and amongst other areas was based on four underpinning principles as shown in the picture below:
A summary of the actions arising from this plan include:
- Establishing a dignified and compassionate miscarriage service tailored to the needs of women.
- The provision of paid leave for miscarriage and stillbirth, delivering this within the public sector and calling on the UK Government to make the necessary changes to employment law to make it available for everyone.
- A review of midwifery and health visiting pathways.
- Unexpected pregnancy complications.
- Age thresholds for screening.
- The establishment of a Scottish Institute for Women's Health.
The full list of actions are shown in the picture below:
Northern Ireland
The Primary Care Women's Health Forum has published a toolkit with Developing the Northern Ireland Women’s Health Pathway in Northern Ireland specifically in mind. It recognised the fact that Northern Ireland has some of the longest outpatient waiting lists within the UK. In 2017 GP Clinical Leads in gynaecology were appointed through GP Federations in Northern Ireland, to explore how access to primary care gynaecology could be improved. Initial data suggested 10% of referrals to secondary care were for common gynaecological problems such as long acting reversible contraception (LARC) requests, uncomplicated heavy menstrual bleeding (HMB) and Hormone Replacement Therapy (HRT) / perimenopausal problems.
Also Northern Irelands NI Direct Health and Wellbeing part of their website has a variety of different illnesses and conditions which focus on women's health. Not exclusive but examples include: