There are a number of practical tips that can be given to parents to help alleviate symptoms and reduce the occurrence of reflux. In many cases these will be sufficient to control symptoms until the oesophageal sphincter matures and reflux naturally abates. In addition to practical advice there are a number of specialist infant formulae that can reduce the incidence of reflux.
Practical advice for managing reflux
- Review volume and frequency of feeds.
- Small, frequent feeds are recommended.
- Use 'anti-reflux' teats and bottles (e.g. Dr Brown's).
- Ensure teat flow is not too fast or slow.
- Frequent winding before, during and after feeds.
- Ensure clothing or nappy is not too tight around the abdomen.
- Keep baby upright during feeds and for 30 minutes afterwards.
- Cot wedges can be used underneath the mattress to incline the baby's sleeping position.
- Never use sleep positioners (e.g. rolled towels or pillows) within the cot as it can increase the risk of suffocation.
- Avoid exposure to tobacco smoke.
NICE guidance on reflux and regurgitation in infants
In 2015 NICE produced guidelines for the recognition, diagnosis and management of GORD in infants.15 NICE recommends a step-wise approach to managing symptoms. In formula-fed infants with frequent regurgitation that causes distress:
- Review the feeding history.
- Reduce the feed volumes if excessive.
- Offer a trial of smaller, more frequent feeds whilst maintaining the same total daily volume.
- Offer a trial of a thickened formula.
Anti-reflux formulae
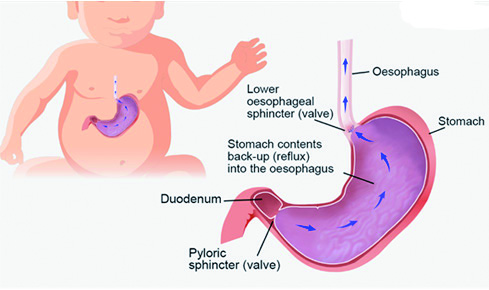
Infants consume comparatively large volumes of liquid and have small stomachs, which puts extreme pressure on the oesophageal sphincter and results in the regular occurrence of reflux. A short oesophagus then makes regurgitation more likely (Figure 6). By increasing the viscosity of the milk it makes it less likely to escape into the oesophagus and so formulae that have been thickened can be recommended to reduce the incidence of reflux and regurgitation.16 These products are known as anti-reflux or anti-regurgitation formulae.
Figure 6:
 Formulae can be thickened in a variety of ways; processed rice, maize starch, potato starch, guar gum and carob bean gum (sometimes called locust bean gum) are all used as thickening agents. A meta-analysis of trial data concluded that thickening agents significantly reduce incidence of regurgitation, reduce some symptoms of GORD and increase weight gain.17 Pre-thickened formulae, such as SMA Staydown and Enfamil AR contain starch as the thickening agent. Studies have suggested that formulae containing processed rice or carob bean gum may produce more viscous feeds compared to starch.18 Aptamil Anti-reflux and Cow & Gate Anti-reflux, both containing carob bean, can reduce incidence of reflux by up to 78% and may help normalise gastric pH.17 Feed thickeners can also be added directly to standard formulae and expressed breastmilk, for example Cow & Gate Instant Carobel.
Formulae can be thickened in a variety of ways; processed rice, maize starch, potato starch, guar gum and carob bean gum (sometimes called locust bean gum) are all used as thickening agents. A meta-analysis of trial data concluded that thickening agents significantly reduce incidence of regurgitation, reduce some symptoms of GORD and increase weight gain.17 Pre-thickened formulae, such as SMA Staydown and Enfamil AR contain starch as the thickening agent. Studies have suggested that formulae containing processed rice or carob bean gum may produce more viscous feeds compared to starch.18 Aptamil Anti-reflux and Cow & Gate Anti-reflux, both containing carob bean, can reduce incidence of reflux by up to 78% and may help normalise gastric pH.17 Feed thickeners can also be added directly to standard formulae and expressed breastmilk, for example Cow & Gate Instant Carobel.
Care must be taken to ensure correct preparation, which should be done immediately prior to use as the milk can thicken further if left to stand. Incorrect preparation, where the milk is over-thickened can cause distension of the abdomen in the short-term and lead to chronic constipation. To reduce the risk of this occurring only one type of thickening product should be used, i.e. Instant Carobel should not be added to anti-reflux milk. The teat size may also need to be increased to ensure proper flow.
Extensively hydrolysed formulae
GORD can be a sign of potential cow's milk protein allergy and when reflux presents in combination with other symptoms such as eczema, erythema and pruritus, CMPA should be considered. Trial of an extensively hydrolysed formula or an amino acid formula if not tolerated, can relieve symptoms and allow a correct diagnosis. Suspected CMPA should be managed as described above, including referral to a GP.
