The skin forms an effective barrier to the penetration of most chemicals including medication. Drugs with a low molecular weight, high lipophilicity and high potency are particularly suited to transdermal administration. The physical characteristics of fentanyl make it suitable for administration via the transdermal or transmucosal route. Low molecular weight and highly lipophilic drugs can pass more easily through the stratum corneum. High drug potency allows a therapeutic effect to be provided by the small volume of drug that can be easily incorporated into a transdermal patch.
Advantages and disadvantages of administering fentanyl transdermally include:
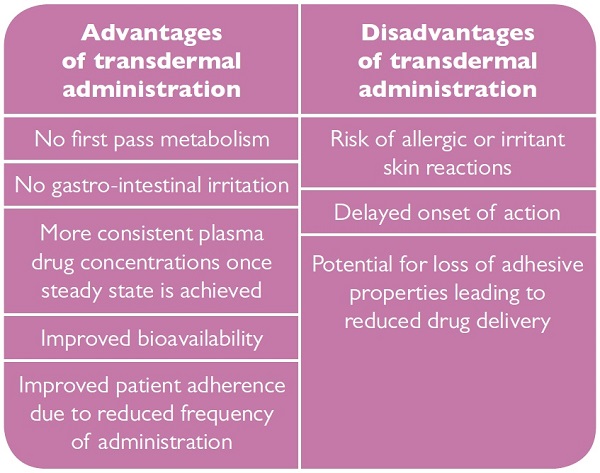
Steady state is usually achieved after approximately 36-48 hours and is maintained until the patches are no longer renewed.7 Avoiding the peaks and troughs associated with conventional drug administration reduces the incidence of breakthrough pain and also side effects such as nausea, vomiting, sedation and also respiratory depression.
On application of a transdermal patch, a concentration gradient is formed. The drug then moves down the gradient from the patch initially into the outer layer of the skin, the stratum corneum, where it forms a second reservoir. It then moves from this reservoir deeper into the skin and into the local vasculature and systemic circulation. This movement of drug down the concentration gradient produces a delay between application of the patch and initiation of symptom relief until the drug reaches therapeutic levels. This delay in pharmacological effect renders patches unsuitable for the treatment of acute pain and requires alternative analgesia for approximately the first twelve hours whilst the patch reaches therapeutic levels.
If transdermal therapy is discontinued a reservoir of fentanyl will remain in the skin providing a continued analgesic effect. This analgesic effect must be taken into account when fentanyl patches are discontinued and an alternative opioid analgesic initiated to avoid opiate side effects such as respiratory depression. It can take approximately sixteen hours (range 13-22 hours) for the serum fentanyl concentration to decrease by 50% after removal of a patch.8 Replacement opioid therapy must be initiated slowly and the dose gradually increased.
Patch application
Fentanyl patches should be applied to a flat area of the upper torso or arm. The area should be dry, clean, hair, oil and lotion free. If necessary, hair should be removed by clipping rather than shaving before application. Patients should be advised that clipping of hair is less likely to irritate the skin than shaving thereby reducing the risk of a topical reaction to the patch. Patches should be examined before application and any patch that appears to be damaged, cut or divided should not be used.
Patches should be replaced every 72 hours, with the old patch always being removed before a new patch is applied. This is to prevent administration of higher than prescribed dose as there will be residual fentanyl in the expired patch. The dose should be titrated depending upon the patient's individual response. Patients using patches in the lower dose range up to 75mcg/hour are usually increased by a 12mcg/hour patch each time, whilst patients with doses in excess of 75mcg/hour will be increased in 25mcg/hour incremental doses. Where necessary, more than one patch can be used to achieve the required dose. It is not recommended to adjust a dose more frequently than every 72 hours.7
Transdermal fentanyl is available as both a reservoir and matrix patch. These patches differ in the mechanism by which the drug is retained within the patch and also how drug release is controlled.
Reservoir patches
Reservoir patches can also be termed a "membrane controlled system" because the drug is held as a gel or solution in a reservoir within the patch with its release being controlled by a rate controlling membrane. Damage to the membrane of a reservoir patch can result in the immediate release of the entire dose and potential overdose. For this reason damaged patches should not be used and reservoir patches should never be cut. Reservoir patches also have an increased potential for abuse as the drug can be more easily extracted from the gel or liquid core. This should be a consideration when choosing the form of patch to be supplied in areas where diversion of medication is a particular problem.
Examples of reservoir patches available in the UK include Tilofyl, Fentalis and Victanyl.
Matrix patches
Matrix patches have the drug incorporated into an adhesive polymer matrix that controls the rate of release of the drug. The dose of drug released is determined by the amount of drug in the patch and the surface area of the patch in contact with the skin.
The advantage of matrix patches is the reduced risk of accidental overdose if the patch membrane is damaged because there is no immediate release of drug. Cutting matrix patches is theoretically safer than cutting a reservoir patch but would still be outside of the product licence. Most manufacturers will advise not to cut patches, primarily because bioavailability studies to determine the effects of cutting a patch on safety and efficacy have not been conducted. The cutting of matrix patches should now be unnecessary with the introduction of the 12mcg/h patch allowing easier dose titration. Matrix patches have a lower potential for abuse as the drug is incorporated into the matrix making it irretrievable.
Matrix patches available in the UK include Matrifen, Mezolar, Durogesic D-Trans, Fencino, and Opiodur.
This demonstrates that matrix patches have clear benefits over reservoir patches in terms of patient safety and reduced potential for abuse and as such, should be the first choice for supply against generic fentanyl prescriptions.
