Diagnosis of angina is dependent on an accurate clinical assessment of the patient including clinical symptoms and trigger factors.
Factors that make a diagnosis of stable angina more likely include1:
- Male gender
- Increasing age
- Established cardiovascular risk factors such as:
- Smoking
- Diabetes
- High blood pressure
- Elevated blood lipid levels
- Family history of premature coronary artery disease (CAD)
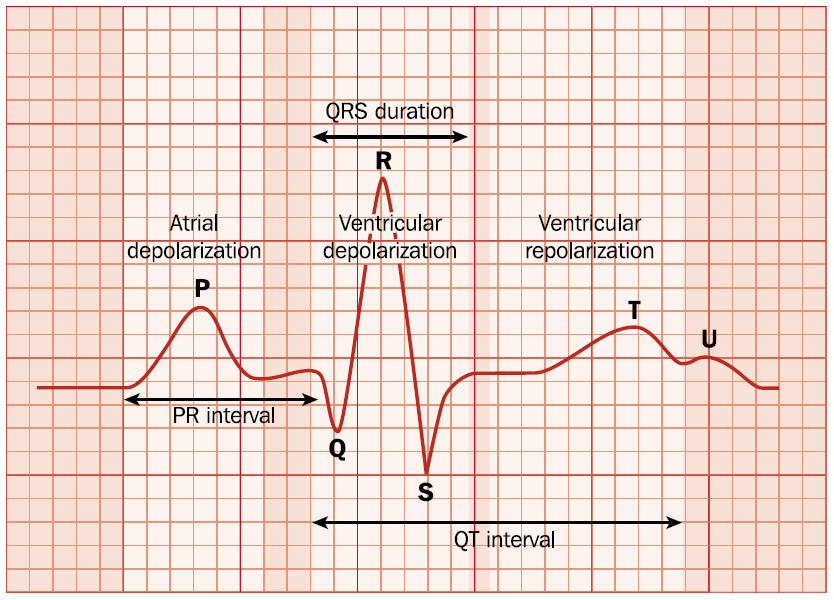
Where the clinical assessment cannot confirm or exclude angina a resting 12-lead ECG should be completed. The ECG will be normal in more than 50% of patients.4 A normal ECG does not exclude a diagnosis of ischaemic heart disease but is suggestive of normal left ventricular function giving a better prognosis for the patient.
Symptoms that would not be consistent with a diagnosis of stable angina include4:
- Continuous or prolonged pain.
- Pain that is not related to any form of activity.
- Pain triggered by breathing.
- Pain associated with dizziness, swallowing difficulties, tingling or palpitations.
- Pain not relieved by GTN.
Differential diagnosis
The chest pain associated with angina can be associated with other medical conditions including:
- Myocardial infarction
- Cardiac arrhythmia
- Gastro-oesophageal reflux disease
- Inflammation of the chest wall
- Anxiety
- Pneumothorax
A myocardial infarction can be differentiated from angina by its trigger factors and also duration. The pain will be more severe and last in excess of 20 minutes whilst angina pain is shorter lived.
Cardiac arrhythmias trigger chest pain that is typically associated with palpitations, breathlessness and transient loss of consciousness.
Gastro-oesophageal reflux disease is caused by acid leaking from the stomach into the oesophagus resulting in a burning pain. The pain of GORD is usually worse when lying down in contrast to angina where symptoms are relieved by rest.
Inflammation of the chest wall results in pain, swelling and tenderness extending over the breastbone and ribs.
Anxiety can manifest as shortness of breath and heart palpitations in addition to chest pain that could be mistaken for CVD. Additional symptoms that are not consistent with angina could include disturbed sleep, reduced appetite, along with a sensation of worry and unease.
Pneumothorax occurs when air leaks into the space between the lungs and chest wall. This produces pressure on the lungs causing them to collapse. Pneumothorax results in a sharp stabbing pain on one side of the chest that is worse on inspiration. Pneumothorax is more common in fit healthy young men while angina is associated with increasing age.
Chest pain could also be associated with fibromyalgia, herpes zoster infection,4 pulmonary embolism, tuberculosis, pulled muscle or pleurisy.
