In OTC
Follow this topic
Bookmark
Record learning outcomes
Whichever way you look at it, the human eye is incredible. It can adjust to movement in milliseconds and is home to the fastest muscle in the body – the orbicularis oculi, which closes the eyelids. Our eyes contain more than 100 million cells, and scientists estimate that they can distinguish between some 10 million colours. This is all the more impressive when you think that they see the world upside down before the brain flips the image.
In simple terms, light enters the eye through the cornea and the lens, which are clear to allow it to pass; the space between them is filled with a watery fluid that maintains eye pressure. Meanwhile, the coloured part of the eye – the iris – controls the size of the pupil, which grows bigger or smaller, depending on the level of brightness, to let more or less light in. The curved cornea then bends the light, forming an upside-down image on the retina, which is packed with photo-sensitive cells. These transform the light into electrical signals, which are transferred via the optic nerve to the brain.
It’s a remarkable organ, but unfortunately things can and do go wrong – from injury and infection to conditions causing sight loss. “Impaired vision impacts drastically on life,” says Alexander Ionides, a consultant ophthalmic surgeon at Moorfields Eye Hospital and lead clinician for Moorfields Private Eye Hospital. “Even having a bit of grit or an eyelash irritating the eye is enough to drive some people beyond distraction.”
Fortunately, there is much that pharmacy teams can do to help patients, from encouraging them to visit an optician, to supporting them with over-the-counter (OTC) products and advice.
Common concerns
Conjunctivitis
With its tell-tale red, itchy and often sticky eyes, conjunctivitis is a condition that’s usually easy to identify. An inflammation of the conjunctiva (the clear membrane that protects the eye) is common in young children, but can also affect adults. It may be caused by an infection (infective conjunctivitis, which is contagious) or an allergy (allergic conjunctivitis, which isn’t), and while not normally serious, it can be uncomfortable.
To help ease symptoms, patients – or, if they’re young, their parents – can gently wash the eyelids using a clean cotton wool pad and water that has been boiled and left to cool. They should start from the inside corner (by the nose) and wipe outwards, using a fresh pad each time and on each eye. It’s also a good idea to wash hands regularly and avoid rubbing the eyes.
In many cases, the problem will clear up in a week or so. However, if treatment is needed, chloramphenicol eye drops or ointment is available from the pharmacy for patients aged two and up. Pharmacy staff should refer if:
- The patient is under two
- They’re experiencing eye pain, vision changes or sensitivity to light
- They’re showing signs of a contact lens allergy, such as bumps on the eyelid
- One or both eyes are very red
- The problem persists for more than a week, or after using OTC eye drops.
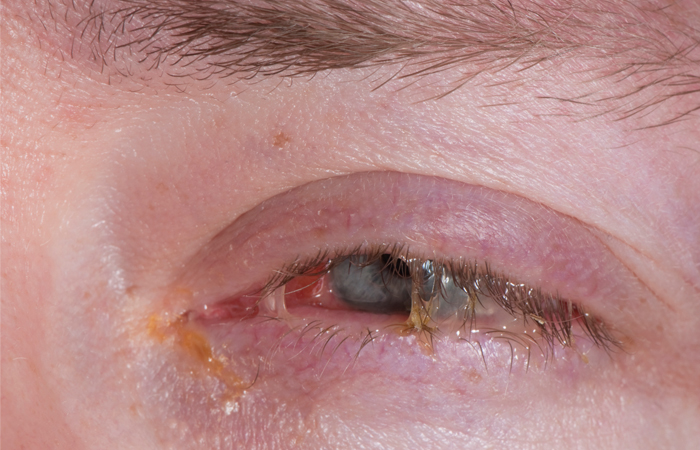
Conjunctivitis is easy to identify with tell-tale red, itchy and often sticky eyes.
Floaters
Patients may describe seeing dots or lines in their vision, known as “floaters,” or flashes of light.
“The bulk of the inside of the eye is made up by vitreous gel, which is about five per cent protein and 95 per cent water,” explains Alexander. “Floaters is the unfortunate term for when the vitreous gel starts to break down and give rise to dots, or strings in the vision. They can appear in all shapes and sizes, such as a ‘net curtain’ billowing in and out of the vision, or ‘cobweb-like’ floaters that can blur the vision intermittently. These do not generally go away, although with time they can move to the periphery or people just get used to them. They are more apparent when looking at a white wall, or blank scenery, a clear blue sky or a well-lit computer screen.”
In most cases, people live with them and nothing needs to be done, he continues, but for some patients “they are so bothersome that they have the vitreous gel removed by surgery”.
The NHS advises that patients should call 111 or see an optician urgently if:
- They are experiencing symptoms of floaters for the first time
- The condition starts or increases suddenly
- They have blurred vision, eye pain, or notice a dark ‘shadow’
- It follows an eye injury or surgery.
Dry eye
The eyes blink more than 10,000 times a day, spreading tear fluid to help keep them lubricated. However, it’s thought that around a quarter of people in the UK experience dry eyes, which can feel sore, itchy, burning or – despite the name – more watery than usual. This occurs when the eyes don’t produce enough tears, or the quality isn’t right, and may be linked to a variety of reasons including age, contact lens use, too much screen time, hormonal changes, environmental factors, and certain medicines or medical conditions such as diabetes, lupus or blepharitis – an inflammation of the eyelid.
The good news is that dry eye is usually straightforward to treat. “Tear drop supplements cannot reproduce the magic of the natural tear film, with billions of years of evolution to create it, but more sprays and drops to supplement it are now available over the counter and online to help with tear film problems and dry eyes,” says Alexander.
Self care tips include taking regular screen breaks, cleaning the eyelids daily, using a humidifier to add moisture to the air, and avoiding smoky or dusty places.
Patients should see their GP promptly if the eye is painful or red, the eyelids change shape, they have extreme sensitivity to light, or they don’t see an improvement after a few weeks of treatment.
Glaucoma
One of the leading causes of blindness, this is the name given to a group of eye conditions that damage the optic nerve. It’s usually caused by a build-up of fluid in the eye, which leads to an increase in pressure. The chance of developing it rises with age, though family history, blood pressure, diabetes and other factors can also increase the risk. Over 700,000 people in the UK have glaucoma, though around half don’t know, according to Glaucoma UK – and the number of those living with it is predicted to increase by 44 per cent between 2015-35.
“There are different types of glaucoma, but by far the commonest is ‘open angle’ glaucoma,” says Alexander. “There are no early warning signs; it is a silent blinding disease that needs to be tested for in those who have glaucoma in the family to pick it up early and start treatment to minimise the visual loss it can cause. This testing can be done by your local optician. Classically, raised eye pressure (different to blood pressure), which is symptomless in the vast majority of people, slowly – over weeks to months to years – damages the nerve fibers that make up the optic nerve and causes irreversible blindness.”
Patients who are concerned about their vision should visit an optician or their GP. Though the damage cannot be undone, early diagnosis can help to prevent it getting worse – with possible treatment options including eye drops to reduce the pressure, laser treatment, or in some cases surgery, according to the NHS. Anyone presenting with symptoms of sudden-onset glaucoma – such as severe eye pain, redness, headache, nausea and/or blurry vision – should be referred to A&E.
“Over 700, 000 people in the UK have glaucoma”
Concerns to watch out for
While some eye issues can be treated at home, there are other circumstances where people should call for an ambulance or go to A&E:
- An object pierces or gets lodged in the eye
- A strong chemical, such as bleach, gets in there (in which case they should also rinse it well with water while awaiting help)
- There is blood or pus coming out, or one/both eyes are dark red
- The patient has a headache, high fever or sensitivity to light
- They can’t move/open the eye.
Cataracts
These are more common in older patients, and usually form gradually. They cause the lens to become cloudy, which then impacts vision. Symptoms may include blurry eyesight, difficulty seeing colours clearly, and problems with glare or bright lights. In the first instance, patients should visit an optician, who may refer to an eye specialist. In milder cases, vision aids can help in the short-term, but the only permanent treatment is surgery, which involves replacing the cloudy lens with an artificial one.
Self care steps for eye health
“Pharmacy teams, as with all healthcare professionals, can encourage customers to take good care of their eye health,” says Mr Ionides. “However, the story is a familiar one. What is good for the heart is good for the brain is good for the eyes. That means avoid diabetes and hypertension and don’t be overweight and sedentary.”
He recommends eating a balanced diet, with plenty of green vegetables and yellow-orange fruits and vegetables, such as squash, orange and red peppers, and carrots. “Oily fish rich in omega-3 are good for the tear film, and vitamin supplements for the eyes may be helpful in giving vitamins A, C and E, as well as zinc and zeaxanthin, lutein and copper, and other trace elements to keep the retina healthy.” He adds that supplements “might be considered in moderation and not for everyone,” and points out that eggs and dark leafy greens (such as spinach and kale) are other healthy sources of lutein and zeaxanthin.
“Try not to smoke and drink too much alcohol as these both increase the risk of cataract and macular problems,” continues Mr Ionides. “While it is not scientifically proven that sunlight causes cataracts, there is some evidence that it might, so sunglasses with UKCA/CE marking can be helpful to protect your eyes and the skin around them.”
Colour blindnes
There are around three million colour blind people in the UK, according to the non-profit organisation Colour Blind Awareness, the majority of whom are male: it affects approximately one in 12 men compared to one in 200 women. This is because the most common forms – collectively known as “red/green colour blindness” – are passed from mother to son on the 23rd chromosome (which is also the chromosome that determines a child’s sex). In some cases, people can also become colour blind as a result of ageing, diseases such as diabetes and multiple sclerosis, or as a side effect of certain medications.
Contrary to popular belief, red/green colour blindness does not mean that people see reds as greens and vice versa, or only can’t ‘see’ red and green. What it does mean is that patients can easily confuse any colours with some red or green element (so, for example, they may confuse blue and purple, because they can’t distinguish the red component of purple). It’s easier to understand this by looking at visual examples, and there are some helpful images on the Colour Blind Awareness website (colourblindawareness.org).
Colour blindness can affect many aspects of people’s daily lives, for example:
- Cooking and eating (e.g. trying to differentiate between food that is rare and well done, or tell different sauces apart)
- Driving and dealing with traffic lights
- Playing sport (e.g. distinguishing between different coloured kits)
- Education, where colour is often used as an important learning tool.
According to Colour Blind Awareness, there is likely to be a colour blind child in each class at school, although it’s not commonly picked up. “Older people will probably have been screened for inherited CVD [colour vision deficiency] at school, but screening at school entry was removed in 2009 and was being phased out well beforehand, so most younger people are not aware they are affected unless it’s in their family,” says CEO and founder Kathryn Albany-Ward. “75 per cent of children have an NHS eye test, but colour blindness does not form part of this test in England and Wales (it does in Scotland), so it’s up to the optometrist’s discretion to test. Most don’t. Our ongoing (unpublished) study shows 80 per cent of children reaching secondary school have never been screened, although 75 per cent have had an eye test with an optometrist.

