In OTC
Follow this topic
Bookmark
Record learning outcomes
Over seven million people in the UK are living with heart or circulatory disease, according to the British Heart Foundation (BHF), who say that an ageing and growing population and improved survival rates from heart and circulatory events could see these numbers rise further.
Data from the BHF shows around four million males and 3.6 million females are living with heart and circulatory diseases in the UK, with the charity estimating that “more than half” of us will get a heart or circulatory condition in our lifetime. Worryingly, these diseases cause around a quarter of all deaths in the UK, equating to 460 a day, or one death every three minutes.
As local, accessible, expert health champions, community pharmacy teams are ideally placed to encourage people to start thinking about their heart health with advice on what the common heart health issues are, and why they could be susceptible to them.
Common coronary complaints
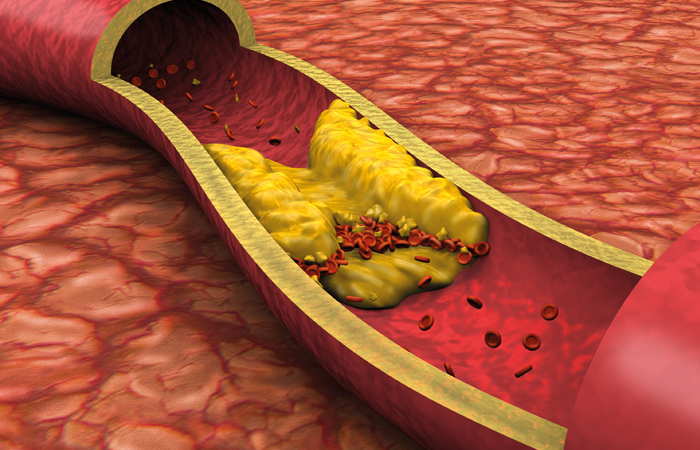
Coronary heart disease (CHD) is the most common type of heart and circulatory disease, and the most common cause of premature death in the UK, according to the BHF. It occurs when coronary arteries become narrowed by a build-up of atheroma, a fatty material within their walls. The pain or discomfort felt from such narrowing is called angina and if a blockage occurs it can cause a myocardial infarction (heart attack).
A heart attack happens when there’s a sudden loss of blood flow to a part of the heart muscle, and without enough oxygen and blood the heart can suffer serious damage. There are around 100,000 hospital admissions each year in the UK due to heart attacks, with more than seven out of 10 people surviving.
Heart failure occurs when the heart is not pumping blood around the body as well as it should, most commonly when the heart muscle has been damaged – for example, after a heart attack. BHF data shows there are around 200,000 new diagnoses of heart failure every year in the UK, with about 80 per cent of diagnoses in England made in hospital, despite 40 per cent of patients having symptoms that the charity says “should have triggered an earlier assessment”. What’s more, the BHF estimates that more than 900,000 people in the UK have heart failure, putting them at two to three times more risk of having a stroke.
The pressure is on
The NHS Community Pharmacy Blood Pressure Check Service supports risk identification and prevention of cardiovascular disease (CVD) by offering anyone a free blood pressure check who:
- Appears to be over the age of 40
- Has not previously been identified as having hypertension or a related condition
- Has not had their blood pressure measured by a health professional within the previous six months.
At the end of a consultation, where readings indicate:
- Low blood pressure: provide appropriate advice and potentially refer the patient to their GP if there are any concerns
- Normal blood pressure: promote healthy behaviours
- High blood pressure: offer 24-hour Ambulatory Blood Pressure Monitoring (ABPM) from the pharmacy and also promote healthy behaviours
- Very high blood pressure: urgently refer the patient to see their GP within 24 hours and inform the GP practice by NHS mail or via another locally agreed platform.
GPs can also refer patients to a participating community pharmacy for either a clinic blood pressure reading or for 24-hour ambulatory monitoring.
Pharmacy advice
Thankfully, pharmacy teams are playing an increasingly important role in giving health advice to customers.
“To encourage heart health, teams should firstly advise people to stop smoking”, says Chloe MacArthur, senior cardiac nurse at the BHF, “and they can also recommend a Mediterranean-style diet, which has been shown to keep your heart healthy. This includes eating plenty of fruit and vegetables, fish and beans, as well as lentils and wholegrains and less processed meat”.
Staying active is also important, with current guidelines recommending at least 150 minutes a week of moderate intensity exercise that gets you warm and comfortably breathless like when walking or pushing a lawn mower.
While this time target can seem daunting, John Bell & Croyden superintendent pharmacist, Reshma Malde, says helping customers work out how to chunk exercise down into smaller increments can make it more achievable. “We can all feel time poor, and not everyone can sign up to a gym membership, so instead encourage people to find ways in their daily life to add in small changes like getting off the bus a stop earlier, which add up to a big change without realising it and all of a sudden they will start seeing the benefits.”
While stress is not directly responsible for heart or circulatory conditions, Chloe says advising people to manage the stress in their life will also benefit them. “This is because stress often leads to unhealthy habits like smoking and drinking alcohol”, she explains, “so to avoid or reduce stress you can recommend exercising to release endorphins, practicing mindfulness or meditation, or simply chatting to friends – and pharmacy teams could also signpost to specialist mental health charities such as Mind”.
As essential members of the wider primary care team, Reshma says the success of any healthcare advice and intervention starts with the connections that pharmacy teams have with their customers. “These are such big topics that can be life changing if they are not zoomed in on”, she says, “but we can change people’s lives in a positive way if we engage and support our patients to lead happier, healthier lives”.
Of course, the bigger picture is that this will also reduce the pressures on the NHS. “Yes, pharmacies are identifying patients with high blood pressure but that can then lead them to contact with GPs, hospitals and specialist clinics, adding to the NHS workload, when this could actually have been caught much earlier,” says Reshma. “If pharmacy teams can stop people becoming what I call ‘a priority’ for the NHS by helping them change some of the elements within their own lifestyle earlier on, we’ll make a bigger impact everywhere else in the system.”
Red flags
“Very high clinic blood pressure (180/120mmHg or higher), or an irregular pulse identify where urgent referrals need to be made”, says Lucy Morris, Numark patient services manager, “but referrals may also need to be made for patients and customers who have a low blood pressure which may put them at risk of falling, or when they feel faint”.
While referral for low blood pressure is less common and most people are asymptomatic, Dr Avinash Hari Narayanan (MBChB), clinical lead at London Medical Laboratory, says: “Symptoms of low blood pressure such as dizziness, light headedness, fainting, blurred vision, fatigue, or confusion, should be referred for further assessment as they may indicate an underlying medical condition, medication side effects, dehydration or even severe acute medical problems such as anaphylaxis or sepsis.”
John Bell & Croyden superintendent pharmacist, Reshma Malde, says pharmacy teams can also look out for red flags for referrals before patients even get as far as Ambulatory Blood Pressure Monitoring. “Maybe they’re already talking about experiencing shortness of breath, pain in the chest, or something as simple getting out of breath if they have to run for a bus and those are all red flags,” she says. “This gives teams a chance to identify potential problems earlier and look into things a bit deeper, engaging the patient with the pharmacy as well as referring them to their GP to give them more joined up care.”
Further information
The BHF has a range of resources to help community pharmacy to provide better information and support to anyone at risk of developing or living with heart and circulatory diseases.
The NHS Heart Age Calculator tool helps people work out how healthy their heart is. The calculator compares your real age to your heart age by asking you questions about your health. It also gives advice on how to improve your heart age by making some healthy lifestyle changes.
“There are around 100,000 hospital admissions each year in the UK due to heart attacks”
Breaking down cholesterol
Cholesterol is a fatty substance produced naturally in the liver, with some coming from the food we eat. It is carried in the blood by proteins and used by every cell in the body.
When cholesterol and proteins combine, they’re called lipoproteins, and there are two main types:
- High-density lipoproteins – known as HDL cholesterol – takes cholesterol back to the liver where it is broken down to be passed out of the body. This is known as ‘good’ cholesterol because it gets rid of ‘bad’ cholesterol from blood vessels
- Non-high-density lipoproteins – known as non-HDL cholesterol – delivers cholesterol from the liver to cells around the body. This is known as ‘bad’ cholesterol because if there is too much it gets stuck to the walls of the arteries. If the arteries that carry blood to the heart get damaged and clogged, it can lead to a heart attack. If this happens in the arteries that carry blood to the brain it can lead to a stroke.
A person’s total cholesterol is their good HDL cholesterol and bad non-HDL cholesterol together. For a healthy heart, the aim is to have a low non-HDL level and a higher HDL level.
How to have healthy cholesterol
A healthy cholesterol level can be maintained through a balance of regular physical exercise, consuming less alcohol, stopping smoking and eating healthy foods.
If someone has high cholesterol, it’s most important for them cut down on foods that are high in saturated fats such as fatty and processed meat, butter, cream, and coconut oil. Swapping saturated fats with foods that are high in unsaturated fat like vegetable oils (sunflower, olive, and rapeseed oil), nuts, avocado and oily fish can help lower blood cholesterol.
“Consuming foods which are high in fibre such as potatoes, pasta, bread or rice will also be beneficial, as well as eating proteins such as beans, pulses, eggs, fish, and meat,” says Lucy. “Another small change that patients can make is to switch out their oils and spreads for unsaturated versions and aim to drink at least six to eight glasses of water per day. Patients won’t need to achieve this full balance with every single meal, but getting the balance right will be really beneficial, and it’s also important to consume less salt, sugar, and saturated fat to keep cholesterol levels at bay.”
Being active also helps the body move the bad cholesterol to the liver where it can be removed out of the body. “Getting blood pumping by being more active will help reduce cholesterol, and it is also crucial to stop smoking,” explains Chloe. “Smoking is not only bad for overall health, but it also makes the ‘bad cholesterol’ stickier and damages the artery walls, making it easier for them to become narrowed or blocked. Smoking also lowers ‘good cholesterol’, which has the job of removing ‘bad cholesterol’. Because of this, smoking
can dramatically increase a person’s risk of heart attacks and stroke.”
Cutting down on alcohol is another way to help the liver work better at removing bad cholesterol, and it may also improve heart health by helping people control their weight and blood pressure.”
In cases where lifestyle modifications alone are not sufficient to maintain healthy cholesterol levels, helping patients manage and optimise their medications has a role to play.
“Pharmacy teams can educate customers about the importance of adhering to prescribed cholesterol-lowering medications,” says Dr Avinash Hari Narayanan (MBChB), clinical lead at London Medical Laboratory. “They can emphasise the significance of taking medications as directed and regularly consulting with their healthcare provider for monitoring and potential adjustments.
“Pharmacy teams can also be a significant point of contact for alternative treatments, supplements and remedies, and will be able to advise and help people remain safe when considering these products. Lastly, pharmacy can help open pragmatic conversations about medications and prescriptions, helping people streamline their prescription logistics, avoid polypharmacy and meet individual circumstances proactively.”