In OTC
Follow this topic
Bookmark
Record learning outcomes
On 8 March 2023, the British Medical Journal (BMJ) published a report stating that the Covid-19 pandemic has had a “minimal” impact on people’s mental health.
The study integrated evidence from 137 studies, comparing mental health, anxiety or depression during the pandemic – including outcomes pre-Covid-19. It found: “No negative changes in mental health at the general population level for general mental health or anxiety symptoms but a minimal worsening of depression symptoms.” Comparatively, these results are stand alone.
Looking at the Health Foundation’s report Unequal pandemic, fairer recovery – the Covid-19 impact inquiry, the idea that mental health was not disproportionately affected by the pandemic couldn’t be further from the truth. Published in July 2021, the study revealed that the percentage of people reporting at least one severe mental health problem doubled from 10.2 per cent in 2017-19 to 23.7 per cent in April 2020, according to figures from the Institute for Fiscal Studies. Furthermore, the Office for National Statistic (ONS) Opinions and Lifestyle survey found that 21 per cent of adults reported symptoms of depression between January and March 2021 compared with only 10 per cent in July 2019 and March 2020.
The extent to which the pandemic has damaged the nation’s mental health is still to be decided, but the thing that remains clear is that mental health is an important issue and an area where pharmacy teams can make significant difference. So, what are the key problems that patients may be facing?
Anxiety and depression
With 7.8 per cent of people meeting the criteria for diagnosis, mixed anxiety and depression is the UK’s most common mental disorder. Furthermore, the ONS found that prevalence for moderate or severe depressive symptoms among adults in Great Britain rose after the start of the pandemic. Symptoms that can be experienced with either condition include:
- Changes in sleep patterns and energy levels
- Trouble concentrating
- Stomach issues with no clear cause
- Increased irritability
- A persistent loop of dark, sad or negative thoughts.
According to the NHS, there are a variety of triggers that could cause a patient to feel anxious or depressed, which can be divided into four categories.
- Work – such as unemployment, redundancy or retirement
- Family – such as relationship difficulties, divorce or bereavement
- Financial problems – such as unexpected bills or borrowing money
- Health – such as illness, injury or increased caring responsibilities.
Stressed out
Stress is another extremely common mental health issues among the UK population. Indeed 74 per cent of people feel so stressed they have been overwhelmed or unable to cope, according to the Mental Health Foundation. Of those, 51 per cent reported also feeling depressed and 61 per cent reported feeling anxious.
The condition can manifest itself in a variety of different symptoms, both physical and mental, according to the NHS.
Physical symptoms
- Headaches and dizziness
- Stomach problems
- Sexual problems
- Muscle tension
- Chest pain.
Mental symptoms
- Difficulty concentrating
- Struggling to make decisions
- Feeling overwhelmed
- Being forgetful.
Help at hand
As part of the community, pharmacy teams are often in the unique position of knowing their patients on a more personal level. Paying attention to what people are talking about and the changes in their mood could make a significant difference to their lives.
If worried about a customer, staff could:
- Signpost them to resources such as the Samaritans helpline (116 123) or email jo@samaritans.org
- Be aware of local community groups and refer any patients experiencing loneliness
- Recommend they speak to family or friends
- Let them know you are always available for them to speak to and unload
- Refer them to the pharmacist or GP to discuss medication or therapy options.
For further information and support, pharmacy teams could also direct customers to online resources including:
- Mind – managing stress
- Every Mind Matters – self-help cognitive behavioural therapy techniques and free Mind Plan.
The kids are alright?
The latest statistics surrounding youth mental health are another area which disputes the BMJ’s report. Indeed, the proportion of 17-19 year olds in England with probable mental health disorders jumped from one in six to one in four from 2021-22 alone, according to Action for Children.
Furthermore, the charity also states 42 per cent of children tell them they now worry about their mental health, a figure that is up from 29 per cent pre-pandemic. Perhaps most shockingly, they reveal, that over a third of parents of children as young as under-five think their child’s long term mental wellbeing will be affected by the pandemic.
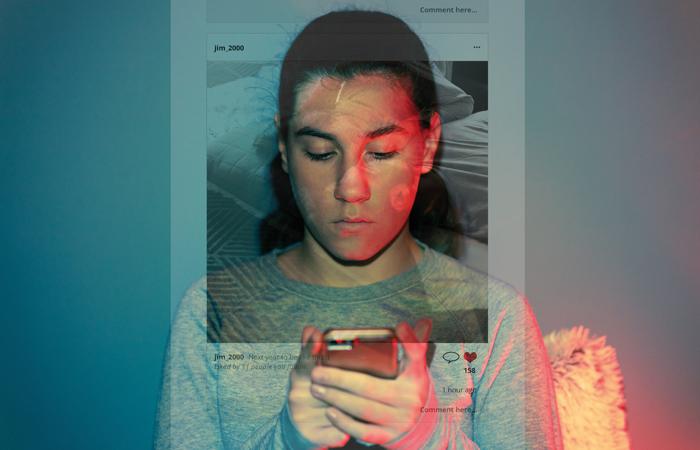
Social media use is considered to be another significant factor in the decline. In fact, teens who spend five hours or more per day on their devices are 71 per cent more likely to have one risk factor for suicide, according to the Priory Group. Additionally, the mental health care organisation states that 52 per cent of students said social media made them feel less confident about how they look or how interesting their life is, whilst one in four teenage girls have edited a photo of themselves because of concerns about body image.
“Social media tricks our brains in a number of ways,” says clinical psychologist Georgia Henderson. “We compare ourselves constantly to our peers to check we ‘fit in’ and ‘belong’.”
Pharmacy staff can alert parents worried about their children’s health to the impact of social media. The Priory Group lists the following as warning signs to look out for in children:
- Appearing worried when receiving notifications
- Keeping their online activity a secret
- Phone use seems to make them angry, sad or frustrated
- Turning off their phone or switches screens when an adult enters the room
- Becoming socially withdrawn.
The organisation also offers this advice for parents worried about their children’s social media use:
- Get to grips with privacy settings – try to understand how apps work and look up any privacy settings or parental controls you could make use of
- Encourage children to talk about their life online – engage your children in discussions about the latest social media trends, or videos that have made them laugh. This increases the likelihood of spotting signs that something might not be quite right
- Introduce some basic boundaries – introduce tech-free zones, such as at the dinner table or at bedtime.
Let’s get technical
Whilst social media highlights the negative effects the digital revolution has had on the general public’s mental health, developments in technology can also have a fairly positive effect for those already suffering, particularly if they are subject to long NHS therapy waiting lists. The 2010s saw an explosion of apps released across different platforms with the sole aim of offering support and resources for a variety of health conditions.
Apps, such as Headspace, are now being recommended by both the NHS and the National Institute for Health and Care Excellence (NICE) as a way for people to have faster access to the therapy and care that they need. In fact, NHS staff themselves have now been given free access to a variety of wellbeing apps including Unmind, Zero Suicide Alliance and Bright Sky.
“Digital technology could transform the experience of people living with mental illnesses,” says Elizabeth Mullenger, lay specialist member on the NICE medical technology advisor committee. “It can be incredibly isolating to be on a long waiting list for in-person treatment.
“Sometimes, people need support in the middle of the night, or after a busy day at work and it’s hard to know where to turn. Having access to digital therapy, can give people the help they need, when they need it. These technologies will allow us to be in charge of our treatment, gaining a sense of autonomy as we navigate our own journey towards positive mental health.”
“Being able to identify problematic thoughts, feeling and behaviours is helpful,” adds Zoë Aston, British Association for Counselling and Psychotherapy (BACP) accredited therapist, mental health consultant and author. “We’ve all been taught to notice changes in our body, on our skin and we know from an early age that physical pain is a sign that something is wrong. So, there is no harm in being able to identify the equivalent for your mental health.”
“NHS waiting lists can be anything between several weeks and a couple of years depending on what the issue is, and a lot can happen in that time, so it’s really helpful to be able to spot symptoms and then know where to go to find the resources to help yourself.”