Lower gastrointestinal problems
In OTC
Follow this topic
Bookmark
Record learning outcomes
Ulcerative colitis and Crohn’s disease are two conditions characterised by inflammation of the gastrointestinal tract. They are chronic, relapsing and remitting, and can result in considerable long-term morbidity

Learning objectives
After reading this feature you should be able to:
• Tell the difference between ulcerative colitis and Crohn’s disease
• Identify the drugs used to treat each condition
• Refer to appropriate patient support groups
Ulcerative colitis is estimated to affect one in 420 people in the UK. It is unclear what causes it, but genetics, environment and immune system factors appear to contribute. People with a first degree relative with the disease have a 10-fold greater risk of developing UC than people with no such relative.
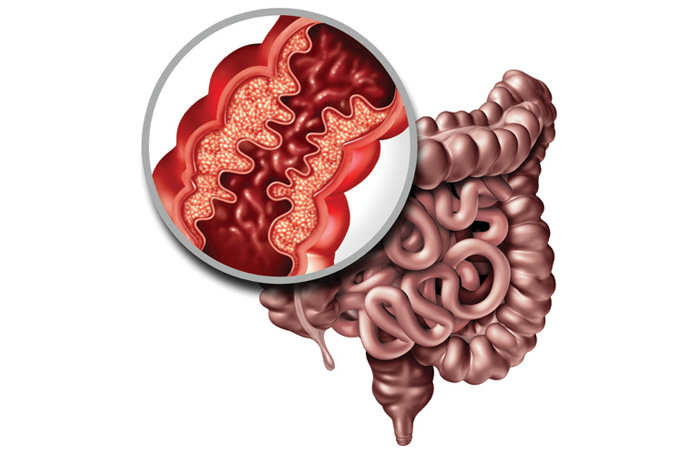
Ulcerative colitis affects the colon and rectum. It causes inflammation and tissue damage to the mucosal and, to a lesser extent, the submucosal layers of the intestine. It is classified according to how much of the intestine is affected. In proctitis, only the rectum is affected, although the sigmoid colon may also be inflamed (known as proctosigmoiditis). In left-sided or distal colitis, inflammation affects the distal colon, which includes the rectum and left side (descending) colon. Total colitis or pancolitis affects the whole of the colon.
In rare cases, ulcerative colitis can cause additional problems in the gut such as strictures, perforations, fistula and toxic megacolon (digestive gases are trapped in the colon causing swelling, pain and tenderness in the abdomen and high fever). Problems outside of the gut, including joint pain, inflammatory conditions of the eyes and skin, thinning bones and increased risk of blood clots may also occur.
Symptoms range from mild to severe and vary in terms of frequency of flare-ups and length of remission from person to person. Flares are characterised by abdominal pain, bloody diarrhoea and excessive watery stools with continuous inflammation and ulceration starting at the distal end of the colon. Loss of appetite and loss of weight also occur.

Crohn’s disease
Crohn’s disease is estimated to affect about one in every 650 people in the UK. Viruses, bacteria, diet, smoking, certain medications and stress have all been suggested as environmental triggers. However, there is no definite evidence that any one of these is the cause of Crohn’s.
Crohn’s can start at any age, but usually appears for the first time between the ages of 10 and 40 years, although there is a small peak in the number of people diagnosed over the age of 60 years. Recent surveys suggest that new cases of Crohn’s are being diagnosed more often, particularly among teenagers and children. The reason for this is not clear. Crohn’s appears to be slightly more common in women than in men. It is also more common in smokers.
Crohn’s can affect any part of the gastrointestinal tract from the mouth to the anus but is most likely to develop in the ileum or the colon. Ulceration can affect all layers of the intestinal wall. Deep ulcers known as skip lesions occur within healthy tissue throughout the intestine. General symptoms of Crohn’s are similar to those of ulcerative colitis (see a summary of similarities and differences in the symptoms and clinical features of the two conditions below).
Symptoms of acute flares include diarrhoea (often with blood and mucus), abdominal pain, loss of appetite and weight loss. Long-term gastrointestinal complications include the development of strictures, fistulas and perianal disease. Extraintestinal manifestations can also occur both during flares and remission with inflammation in the joints, eyes (e.g. scleritis and uveitis) and skin (blisters and red swellings).
Patients with both Crohn’s and ulcerative colitis have an increased risk of colon cancer, particularly if they do not adhere to treatment.
Recent surveys suggest that new cases of Crohn’s are being diagnosed more often, particularly among teenagers and children
Drug treatment
The main types of drugs used in ulcerative colitis and Crohn’s disease are aminosalicylates, corticosteroids, immunosuppressants and biologics. Loperamide hydrochloride or codeine phosphate can be used to manage diarrhoea associated with Crohn’s disease in those who do not have colitis. Colestyramine is licensed for the relief of diarrhoea associated with Crohn’s disease.
Aminosalicylates (5-ASAs)
Aminosalicylates (e.g. mesalazine, olsalazine, balasalazide, sulfasalazine) are used to treat mild to moderate ulcerative colitis flares and in the maintenance of remission. Mesalazine is the most commonly used. Topical formulations (e.g. suppositories)are recommended first-line in patients with initial presentation of mild to moderate or inflammatory exacerbations in proctitis, proctosigmoiditis, left-sided ulcerative colitis and extensive colitis, and for maintenance of remission.
Oral preparations can be used in patients who prefer not to use enemas or suppositories or if remission is not achieved within four weeks. When used to maintain remission, single daily doses of oral aminosalicylates can be more effective than multiple daily dosing, but may result in more side-effects.
The BNF states that there is no evidence to show that any one oral preparation of mesalazine is more effective than another and the choice depends on patient preference. In addition to therapeutic benefits in ulcerative colitis, aminosalicylates have been shown to reduce the risk of colon cancer.
Aminosalicylates are not generally recommended in Crohn’s disease due to lack of evidence for efficacy but they may be preferred in acute flare-ups because they have fewer side-effects than corticosteroids. They are no longer recommended to prevent flares following surgery for Crohn’s disease.
Key facts
Community pharmacists can play a key role in supporting patients with inflammatory GI conditions by:
• Getting to know the individuals who suffer with these chronic conditions
• Offering advice on the importance of treatment adherence and monitoring
• Providing lifestyle information.
Corticosteroids
A corticosteroid (e.g. prednisolone, methylprednisolone or intravenous hydrocortisone) is used to induce remission in patients with a first presentation or a single inflammatory exacerbation of Crohn’s disease in a 12-month period.
A topical or oral corticosteroid for four to eight weeks should be considered for patients in whom aminosalicylates are not suitable. Current guidelines recommend a course of prednisolone 40mg daily reduced by 5mg weekly. Doses of <15mg daily, faster reduction regimens or shorter courses are ineffective in controlling a flare.
Corticosteroids have no proven efficacy for maintenance of remission and should not be used for this purpose. The risk of side-effects including bone thinning and hyperglycaemia increases with prolonged use (defined as requiring a repeat course within three months or continuous use for longer than three months).
Corticosteroid dependency (where the patient experiences flares when the dose is reduced or stopped entirely) occur in 10-20 per cent of patients. Calcium and vitamin D should be co-prescribed to reduce the risk of osteoporosis.
Rectal preparations are less acceptable to many patients but are effective, especially in distal disease. Enemas penetrate further in the colon than rectal foams but are less acceptable to patients. Suppositories are more effective than enemas in proctitis.
Hospital admission is required in patients with acute severe disease and treatment with intravenous hydrocortisone will be given often with the addition of infliximab or ciclosporin. Surgery is considered if there is little or no improvement within 72 hours of starting intravenous corticosteroids or where symptoms worsen despite treatment.
Immunomodulators
Thiopurines (e.g. azathioprine and mercaptopurine) are the first-line immunomodulators used for the treatment of inflammatory bowel disease. The aim is to maintain remission if there are two or more inflammatory exacerbations during a 12-month period that require treatment with corticosteroids or where remission cannot be maintained with aminosalicylates.
Methotrexate is another option for maintenance of remission in Crohn’s disease in patients who required the drug to induce remission or who are intolerant or not suitable for aminosalicylates.
Azathioprine is a prodrug that is metabolised to mercaptopurine, which in turn is metabolised by a series of enzymes into pharmacologically active thioguanine nucleotides (TGNs). Mercaptopurine is metabolised by the enzyme thiopurine methyltransferase (TMPT) to produce methylmercaptopurine (MeMP) and xanthine oxidase, neither of which is pharmacologically active. High levels of TGN can produce dose-related side-effects such as myelosuppression. Patients with high levels of TMPT can produce high levels of MeMP, which cause liver toxicity.
TMPT levels should be measured before a patient starts on a thiopurine and the starting dose adjusted. TGN and MeMP levels should also be monitored to optimise outcomes and/or if the patient is not responding to treatment.
Biological drugs
Biologics are the newest group of drugs used to treat inflammatory bowel diseases. Anti-TNF drugs, such as intravenous infliximab, subcutaneous adalimumab and golimumab target tumour necrosis factor, preventing inflammation. They are effective at inducing remission in people with severe active disease which has not responded to conventional therapy, or where conventional therapy is not tolerated. These drugs are also effective at maintaining remission. Therapy may be optimised by using therapeutic drug monitoring of drug levels and antibody levels.
Ustekinumab and vedolizumab are monoclonal antibodies. They are recommended by NICE within their marketing authorisation as an option for the treatment of moderate or severe ulcerative colitis and Crohn’s disease. They should be used only when anti-TNF drugs have failed or are contraindicated or cannot be tolerated. The manufacturer must provide these drugs with the discount agreed in the patient access scheme.
Prescribing of biologics is always part of a shared care protocol with treatment and initial prescribing and monitoring conducted in specialist centres.
Irritable bowel syndrome
Irritable bowel syndrome (IBS) is a common, chronic and often lifelong condition. It mainly affects people between 20 and 30 years of age. It is more common in women. Symptoms include abdominal discomfort or pain, diarrhoea, constipation, urgency, straining with incomplete evacuation, bloating and passage of mucus. Symptoms are often relieved with defaecation.
Treatment of IBS is focused on symptom control to improve quality of life. The BNF states that diet and lifestyle changes including regular meals, increased physical activity and limiting fresh fruit to no more than three portions a day can be recommended. Fibre intake should be reviewed. If an increase in fibre is required, the focus should be on soluble fibre (e.g. oats, ispaghula husk) and intake of insoluble fibre (bran) and resistant starch discouraged.
Fluid intake should be increased to at least eight cups daily (mostly water) with a reduction in caffeine, alcohol and fizzy drinks and avoidance of the artificial sweetener sorbitol. If symptoms persist, single food avoidance and exclusion diets may be recommended by a specialist dietitian. Probiotics are sometimes used.
Drug treatments, many of which are available over the counter, include antispasmodics (alverine citrate, mebeverine hydrochloride, peppermint oil), laxatives to treat constipation and loperamide to treat diarrhoea. Patients with moderate or severe IBS with constipation who have not responded to laxatives and have suffered constipation for at least 12 months can be treated with linaclotide.
Main similarities and differences between ulcerative colitis and Crohn’s disease
Similarities
• Both conditions often develop in teenagers and young adults although they can occur at any age. The peak age of diagnosis is 15-25 years with a second peak at 50 years
• Ulcerative colitis and Crohn’s disease affect men and women equally
• The general symptoms of ulcerative colitis and Crohn’s disease are similar (e.g. diarrhoea, sometimes with blood and mucus, abdominal pain, tiredness and fatigue, anaemia, loss of appetite and weight loss)
• Both can cause additional problems in the gastrointestinal tract (e.g. strictures, perforations and fistulas)
• Both can affect other parts of the body, including the joints (arthritis), eyes (scleritis and uveitis) and skin (blistering and painful swelling), loss of hair, often during a flare although they can occur during remission
• Both conditions increase the risk of colon cancer particularly if treatment adherence is poor
• Both conditions are linked with increased risk of blood clots (including deep vein thrombosis) and thinning bones
• The causes of both ulcerative colitis and Crohn’s disease are unclear
• Both conditions have similar types of contributing factors such as environmental, genetic and immunological factors
• The effects of diet on both conditions are unclear and poorly understood.
Differences
• Ulcerative colitis affects the colon and rectum, while Crohn’s disease can occur anywhere between the mouth and the anus
• Ulcerative colitis causes inflammation and tissue damage to the mucosal (inner layer) of the colon and rectum. Crohn’s disease can affect all layers of the intestinal wall
• Symptoms of an acute ulcerative colitis flare include excessive watery stools, bloody diarrhoea, with continuous ulceration and inflammation starting at the distal end of the colon. Symptoms of an acute Crohn’s disease flare include abdominal pain and diarrhoea, often with blood, mucus and weight loss
• Additional problems in the gastrointestinal tract are more common in Crohn’s disease
• One in 25 people with Crohn’s disease are estimated to suffer from mouth ulcers, usually when the condition is active
• Smoking appears to be associated with double the risk and severity of Crohn’s disease, but seems to be protective in ulcerative colitis.
Information for patients with inflammatory bowel disorders
- Explain that an inflammatory bowel disorder is a lifelong condition, which may have unpredictable relapses and remissions. Specialist drug treatments aim to induce remission of the disease and to treat symptoms. Occasionally surgical intervention may be necessary
- Encourage healthy lifestyle measures, including maintaining a healthy weight and taking regular exercise if possible
- Watch for unintended weight loss
- Stopping smoking is important in patients with Crohn’s disease
- Explain that most women with Crohn’s disease or ulcerative colitis will have normal pregnancies and healthy babies. Some research has linked these conditions with pre-term and low birth weight babies so advise pregnant women to keep all appointments for antenatal care
- Consider risk of osteoporosis. Advise on dietary calcium and ensure co-prescribing of calcium and vitamin D
- Ensure follow-up has been arranged with a gastroenterologist and/or specialist nurse if appropriate, and encourage the person to attend appointments regularly
- If a patient is taking immunosuppressant or biologic drugs, ensure they are aware that:
- Live vaccines are contraindicated so they should only be given before the start of specialist treatment, or else postponed for at least six months after stopping this therapy
- They are at increased risk of influenza and pneumococcal infection and should receive appropriate vaccinations regularly
- Ensure patients are aware of the need for colorectal cancer surveillance and have colonoscopy screening arranged by the specialist team if diagnosed with IBD 10 years ago or more (with the exception of those with confirmed proctitis alone)
- Ensure that children and young people have their growth (height and weight) and pubertal development monitored regularly.
Patient support groups
• Crohn’s and Colitis UK is a national charity that provides support for people with ulcerative colitis and Crohn’s disease and their families. It provides a range of information sheets and booklets on managing symptoms, drug treatments, diet, pregnancy, education, employment and travel.
• CICRA: Crohn’s in Childhood Research Association is a national charity that supports children and young people with inflammatory bowel disease and provides patient information and young people’s forums for peer support.
